In March’s Science in the News, Tiffany, Lindsey and Jon
used a hypothetical example of some sick students at a school to discuss what
outbreaks are, what can cause outbreaks and how we can protect ourselves. In
real life, disease detectives – more formally known as epidemiologists – do
many things to help detect, track and prevent disease outbreaks. Some work
directly with patients or communities, collecting samples for analysis and
helping administer health policies (such as vaccination campaigns). Others are
based at organizations such as the Centers for Disease Control and Prevention
(CDC) or pharmaceutical companies. They may work as administrators or work in
labs.
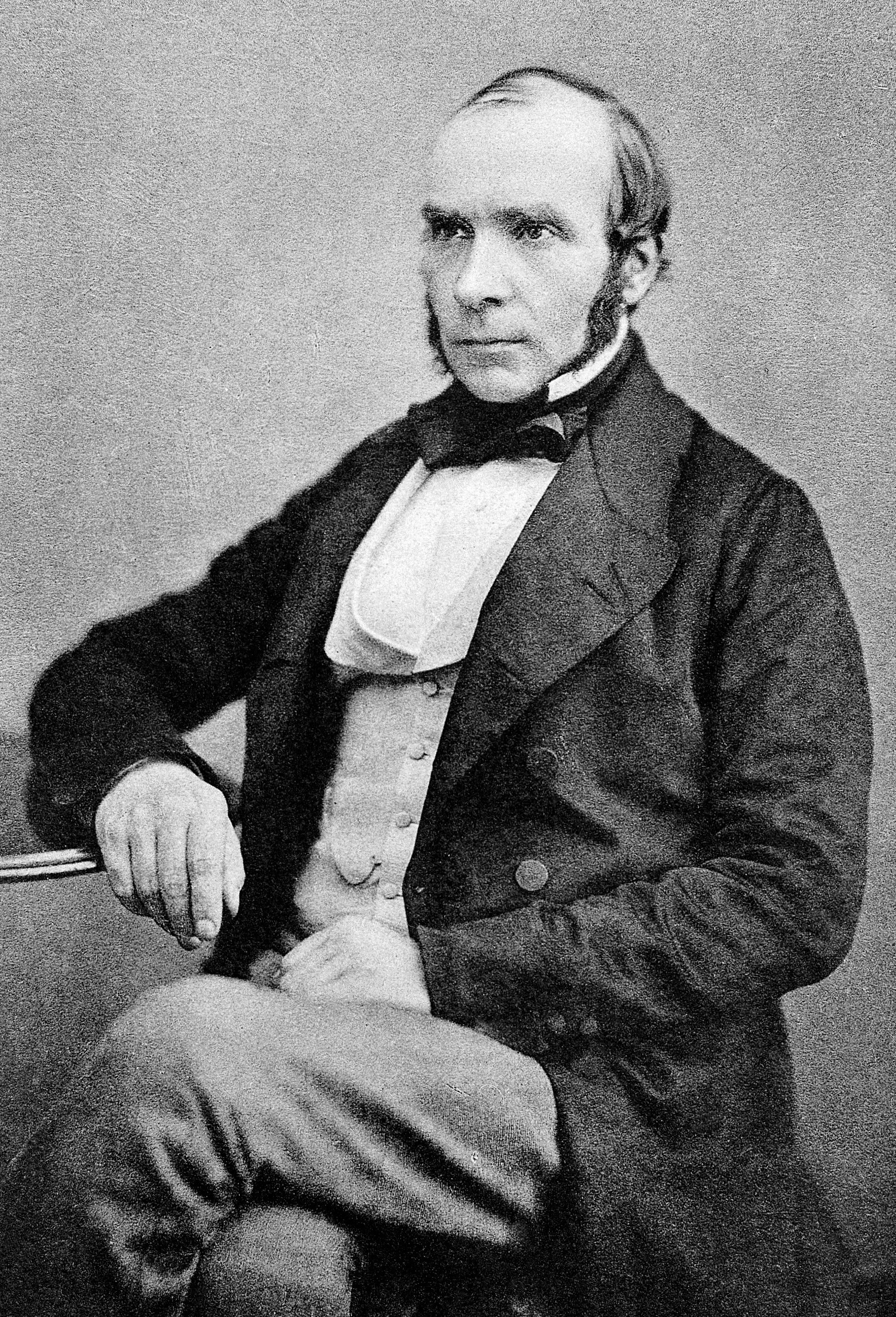

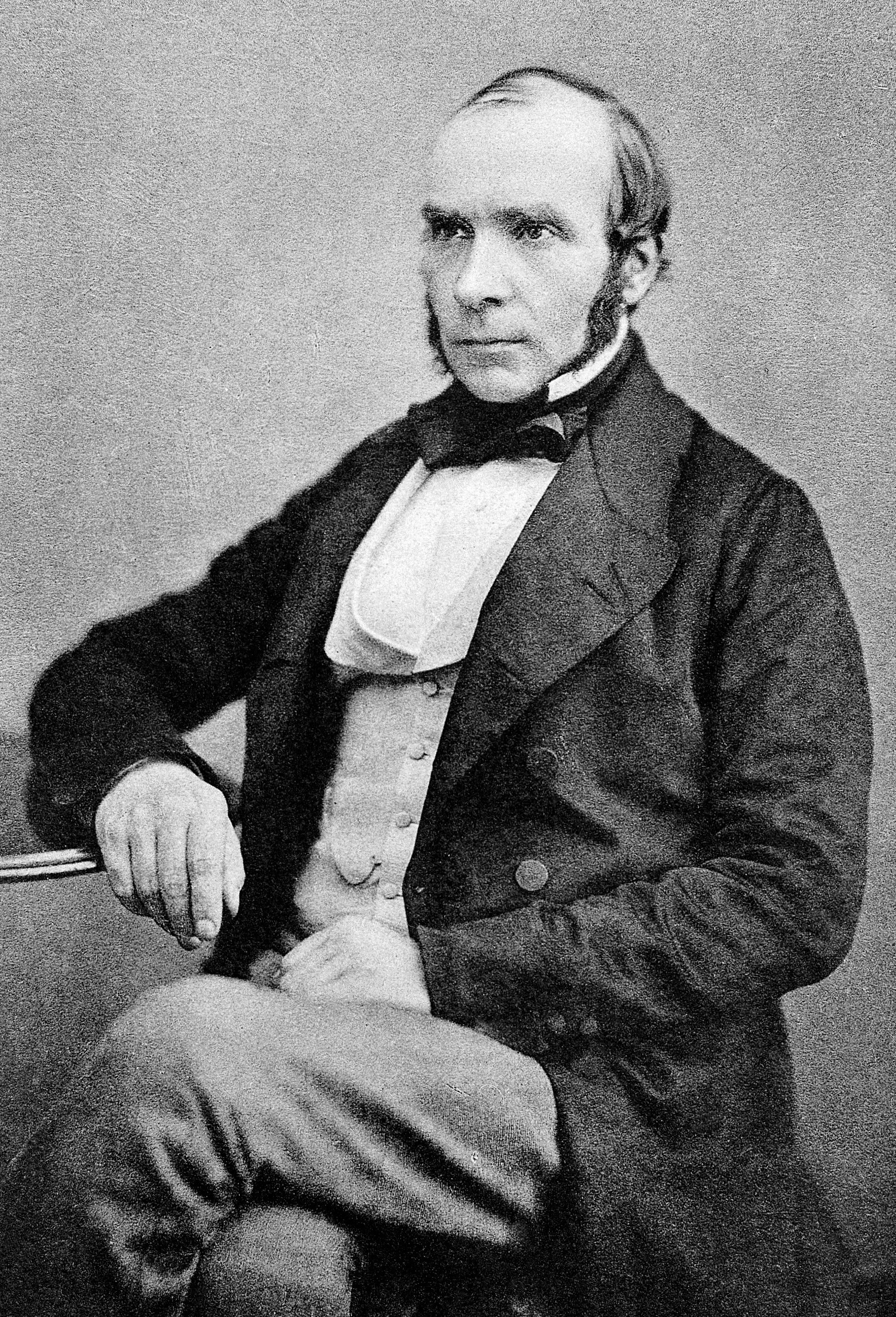

John Snow, the "father of epidemiology" (not to be confused with Jon Snow from Game of Thrones!).
Sources: http://en.wikipedia.org/wiki/File:John_Snow.jpg
http://sharetv.org/shows/game_of_thrones/cast/jon_snow
When did epidemiology get started? The “father of
epidemiology” is often considered to be Dr. John Snow, who determined the cause
of a cholera epidemic in London in 1854. Cholera is caused by the bacteria Vibrio cholera, which infects the small
intestine, leading to watery diarrhea and vomiting. Without proper treatment,
it is often fatal. Historically, cholera epidemics have been both frequent and
devastating due to poor sanitation and they continue to occur in less developed
parts of the world (in the wake of the 2010 earthquake, Haiti experienced a
cholera outbreak that resulted in over four thousand deaths). During the 1854
cholera epidemic, Snow interviewed people to determine where cholera cases had
occurred and found that many of them clustered around one water pump. He was
further able to demonstrate that areas in the city that exclusively relied on
this pump had the most cholera cases. His breakthrough was particularly
impressive given that disease transmission was still poorly understood – most
people, including most scientists, believed that people got sick through
breathing “bad air.” Nobody knew that bacteria could cause diseases. Snow,
perhaps unintentionally, set a precedent for evaluating future outbreaks
although his belief that disease was not caused by the air was dismissed in the
immediate aftermath of the 1854 epidemic.
 |
This map shows how the cholera cases were clustered in the 1854 epidemic.
Source: http://en.wikipedia.org/wiki/File:Snow-cholera-map.jpg
|
If you’re interested in learning more about the history of
epidemics, you might be interested in the following course “Epidemics in
Western Society since 1600” (offered here, free, for either video or podcast
downloading).
Given the broad range of activities epidemiologists carry
out, how does one become an epidemiologist? Epidemiologists are often, but not
always, doctors. Non-physicians generally have graduate degrees in epidemiology
or public health. Yale has one of the oldest schools of public health in the
country (founded in 1915). To find out more about epidemiology and public
health research at Yale, check out the School of Public Health’s website.
Changing topics a little, I wanted to expand a bit on two
types of tests that Jon mentioned can be used to detect norovirus and
rotavirus. Viruses contain DNA or RNA cores protected by a protein shell. Viruses
are super tiny and therefore epidemiologists need to use indirect methods to
detect their presence. One test is polymerase chain reaction (commonly
abbreviated as PCR). In this test, short pieces of DNA (called primers) are
used to amplify a known viral gene. If viral DNA is present, the primers will
stick to the gene of interest. By using a special enzyme, this gene can then be
copied. This stick and copy reaction will be repeated many times. In each
repeat there will be exponentially more copies of the gene available for
amplification. In this way, you can generate a sufficient amount of DNA to
detect and measure.
 |
| Source: Saheli Sadanand |
Another test that can be used to indirectly assess the presence of virus particles is an ELISA, which stands for Enzyme-Linked Immunosorbent Assay. Although the name makes it sound complicated, it’s actually quite straightforward. In this assay, you are trying to detect antibodies, proteins that our immune system makes to bind to and get rid of pathogens such as viruses and bacteria. To do this, you basically construct a sandwich. In the norovirus and rotavirus example, the bottom layer of the sandwich are virus particles. You then load your sample of interest (for example, blood from the sick patients). Then you add a detecting reagent, which is another antibody – but specific for the non-virus-specific portion of the antibodies. Finally, you add a special chemical that reacts with the detecting reagent to produce a color. The brighter the color, the more virus-specific antibodies that are present in the sample. With the appropriate controls (for example, a sample that comes from a healthy person), epidemiologists can determine whether the amount of virus-specific antibody is abnormal – which would imply that the patient is in fact sick with the virus.
-Saheli Sadanand
5th year Immunobiology graduate student
No comments:
Post a Comment